By Alison Laurio, News contributor
Dean Wolf has spent his entire working life as a social worker in the field helping others. Now he is asking others to help him, and said it is not an easy thing to do.
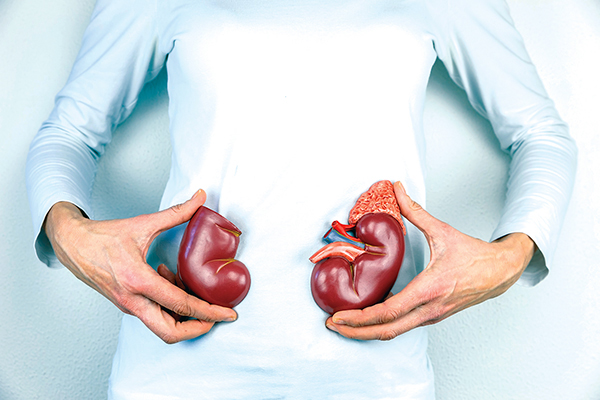
Even though there are more than 200,000 Americans living
with a kidney transplant, the National Kidney Foundation says
on average, 3,000 new patients are added to the kidney waiting
list every month. And 13 people a day — or 4,745
people a year — die while waiting for a kidney.
“As much as I have empathy for people, I need a kidney,” he said it is not an easy thing to do. Wolf, 67, was diagnosed with Type 2 diabetes in 1997. He was diagnosed as having kidney failure about 10 years ago, and he had robotic heart bypass surgery in 1997. He now is in end stage renal disease (ESRD) but is not on dialysis.
He’s still working every day at his family practice, Rhizome Connections, although he says he’s tired a lot, sometimes suffers from nausea and doesn’t have the stamina he once had. Some days he “feels like a wet noodle.”
Wolf is on the United Network for Organ Sharing list, a waiting list for deceased kidneys that the federal government operates. Neither Wolf’s wife nor his 25-year-old son, nor any other relative, is a match for living kidney donation. Because of his background, Wolf believes a living donor would be best for him.
It wasn’t until he connected with Harvey Mysel, founder and president of the Living Kidney Donors Network, that Wolf gathered the courage to go public with his need.
“A lot of people don’t know what to do,” Mysel said. “People don’t want to ask. I tell people it’s like networking. Even if you don’t ask, tell your story. If you’re effective, people know what you need.”
Wolf is among hundreds of thousands of people in the U.S. who are waiting for kidneys or other organs.
The National Kidney Foundation says on average, 3,000 new patients are added to the kidney waiting list every month, and 13 people a day — or 4,745 people a year — die while waiting for a kidney.
Nephrology Social Work
Social workers who work in this area say they fill many roles, such as educating patients and their families, providing counseling, developing care plans and focusing on a good quality of life for their patients.
Andrea Dekam, a nephrology social worker at the University of Michigan Dialysis Clinic in Livonia, Mich., describes her job as being a “Jack of All Trades.”
“Nephrology social workers do a little bit of everything” and are an integral part of interdisciplinary teams, she said. “We work with both adult and pediatric populations depending on the position. We often follow patients from the beginning to the end of their disease process.”
That includes performing routine psychosocial assessments; developing care plans; and providing screenings, counseling and referrals to address mental health concerns, Dekam said.
“Patients often experience difficulties with adjustment to illness, sometimes resulting in feelings of depression or anxiety,” she said. “Many NSWs are utilizing skills learned in the Symptom-Targeted Intervention program to help address issues related to mental health and adherence.”
They also educate patients and their families on treatment options, advance directives and resources, said Dekam, LMSW, NSW-C and executive committee chair of the Council of Nephrology Social Workers.
“We provide ongoing support and encouragement to help patients maintain a good quality of life,” she said. “I think an important issue that often comes up is one’s coping or adjustment to illness. Research has shown that at any given time, 20 percent to 40 percent of the dialysis population is experiencing some level of depression. NSWs are the ones equipped to address those feelings.”
Other tasks include helping with fluid control, dietary issues, medication compliance, adherence to treatment regimen and end of life. They support the patient’s vocational goals, encouraging them to stay working, and they can serve as an advocate with employers as needed, Dekam said.
“We also help with tangible concerns related to housing, transportation, financial problems and prescription issues like coverage and cost,” she said. “Dialysis and transplant social workers work in collaboration in helping patients navigate the transplant process.”
“We solely provide the psychosocial support necessary for many patients to cope with their disease and treatment. NSWs have the ability to develop long-term, therapeutic relationships with patients due to the nature of their disease. This aids in building rapport, proper assessment and individualized interventions.”
From the April 2017 NASW News. Read the full story here.